21st July 2020
Tomorrow I re-enter the world of work. Exciting? Yes. Daunting? Absolutely…

In fact I’m terrified. I left work on the 21st November 2019 with absolutely no idea that it would be 8 months before I stepped back into the building, and my goodness so much has changed since then. I guess we are both very different now, me and the surgery.
It’s not like maternity leave, where you change but the systems you work in largely stay the same. I am returning to a GP land completely different to what I left. I fear I am going in very much on the back foot. My colleagues have had the “advantage” of living the changes Corona has brought about. I am having to learn so much. There has been an information explosion in the last 4-5 months. There is no other description for it. I have read and re-read national and local Covid guidance and protocols, but until I am back in the throes of work it all seems a little abstract and hard to apply.
Since the bowel cancer diagnosis in November, I feel rather like I have been living in some parallel, surreal universe. And since finishing treatment prematurely in March, I guess everything has been gearing up towards this point – the return to work. The ultimate step in my journey towards “new normal”. A term, that now, thanks to Corona, I suppose we’re all experiencing some form of.
These last couple of weeks, I have found myself reflecting on all that has happened over the last 8 months and how life has changed. Obviously the bowel cancer diagnosis itself was pretty devastating, but it’s not all been bad…
One undoubted benefit has been the amount of time I have been able to spend with my family, initially courtesy of cancer and treatment, and, latterly, thanks to Covid. I have simply loved spending so much time with my husband and three children. Homeschooling has had its challenges but all the mealtimes, walks, and conversation we have shared have been a blessing. I feel I have got to know my children better throughout this experience.

I have been given the opportunity to re-evaluate what is important in life and address the work-life balance. I thought I had it sorted before all this happened – I was wrong.
Latterly (definitely not in the early weeks!), I have slept more and better than ever before. I’ve learnt I need more sleep. While I can get by on five hours sleep a night, I am definitely a generally better person for at least eight!
While by no means a grand master in it, I have also been learning the art of patience. This has never been a particular strength of mine. I like things to be done, and usually by yesterday. I have had lots (and lots) of practice in recent months – nothing after all has really gone to plan. In this process I have, I think, learnt to be a more patient patient.
I have also learnt how stressful it is to be a patient at times, especially as a doctor patient, and how frustrating it is not to be in the possession of knowledge – something as doctors we are so used to being.
I have found support and wisdom in unexpected places. Social media has made it possible to connect with other doctors going through or having gone through cancer. With so many of the normal cancer support services being unavailable in recent months, these groups have been an absolutely invaluable resource.
My love for General Practice, and in particular face to face consultation has deepened, but I am anxious about the land I am returning to. Telephone triage has long been an established part of GP, but face to face consultation historically has been the mainstay. Since lockdown I have really struggled with the vast majority of my clinical care being telephone based. The doctor-patient interface has been completely transformed by Corona and made us see what is possible in these exceptional circumstances. It will undoubtedly lead to long overdue, and welcome efficiencies within primary care, and across healthcare as a whole. However the absence of face to face interactions in my clinical care has highlighted to me the importance of presence in a doctor-patient interaction.
It has made me realise how rich and nuanced General Practice is, and the incredible depths of face to face interaction. I now really appreciate the value of such a sensory-rich encounter, having been on the other side of the fence. It is never just about the verbal content of the exchange – consultations are laden with so much non-verbal information that just doesn’t come through on the telephone, or even video – information gained by both doctor and patient. I have really valued speaking to my oncologist on the telephone throughout this lockdown, but it has been hard relying on just the audio input. I also find it so strange to think I was referred to a specialist who I had two telephone consultations with – someone I’ve never met, and someone I will probably never see. This would have been unthinkable 6 months ago.
I hope the core, the essence, of General Practice consultation, isn’t lost in the post-Covid revolution.
There are still challenges for me. I’ve talked before about anger. Counselling has helped somewhat. I realise increasingly just how angry I’ve been about the whole situation. While the intensity has abated, it is still there. That one fire engine is still in attendance, constantly damping down. I can’t discharge it back to the station, not yet.

I still struggle with the erosion of control throughout this period, although I am trying to shift the focus away from what I can’t, and towards the many facets of life I still can exert control in.
Acceptance of all that has happened is still a real challenge – the diagnosis, the year-long pre-amble, everything. I guess (and hope) time will help in this respect.
For me, now, one of the biggest difficulties is figuring out how I navigate the next three years. If mets or recurrence is going to happen, that’s when it is most likely to occur. I know I will get through somehow, but I don’t want to be living with the sword of Damocles constantly dangling over my head.
I have all my eventualities planned out in my head. This has been a necessary part of my coping strategy – but the drawback is the emotional exhaustion in carrying around that “readiness”. I’ve come to the conclusion that I need to put my “readiness” for that particularly rubbish outcome, if it should happen, in a metaphorical “emergency box”. At the moment, that box is tightly clutched in my arms. I just can’t put it down yet. I’m tired and my arms are aching. I want to reach a point where I can put that box down, move it aside while still in sight, and give my arms a rest. It’s a work in progress, but I’m getting there.
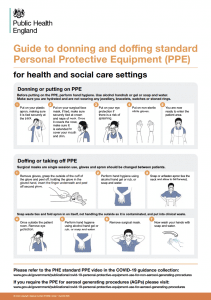
So tomorrow awaits, who knows what challenges it will bring. The superwoman cape that’s been hanging in the cupboard will be replaced with scrubs and PPE for now, but I might still take it with me just in case… who knows, it might come in handy.

Good luck xxx
Your landing Claire will be fine i am sure as you seem to have prepared for it so well. Fire engines are only there to be called on for emergencies and we all need those.Prayers for you that all will be well tomorrow and in the foreseeable future.
Love and best wishes
Tony
Much of this resonates so strongly with me. I also felt I needed to try and prepare myself for recurrence or mets. It is exhausting. Slowly, with time (and a few negative scans), it is now a small part of my thinking. Best wishes Deb